- Joined
- Jun 8, 2008
- Messages
- 56,727
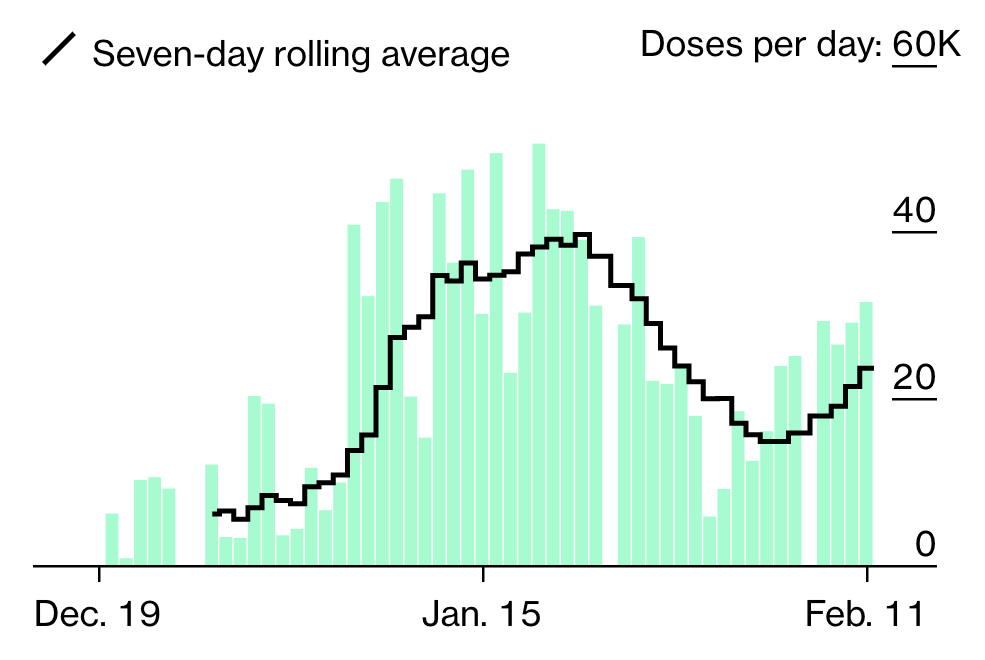
Am I understanding correctly that it has not been determined that a COVID vaccine prevents transmission and it also hasn’t been proven that it keeps someone vaccinated from catching COVID? In this interview she says “in the event that they prevent COVID”. The WHO said the same in December and Fauci himself said this just last week.
They keep on talking about herd immunity but there won’t be herd immunity if the vaccines don’t prevent transmission of the virus.
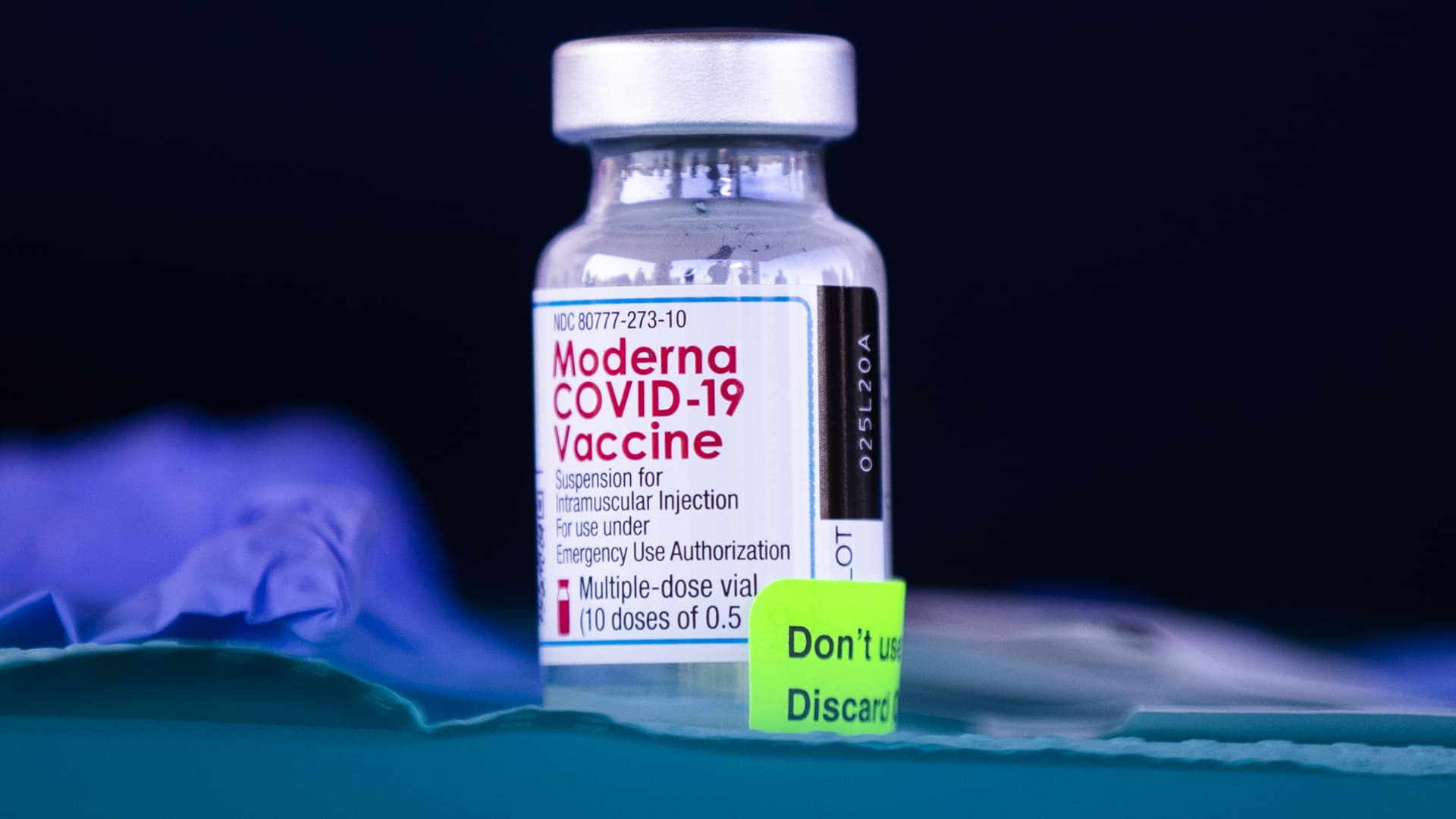
We don’t know yet (too soon) if it helps prevent transmission. It probably does help decrease it imo. But time will tell. And the Pfizer and Moderna vaccines are up to 95% effective in preventing infection after one has received both doses and two weeks from the second dose have passed. I’m talking in general terms only. YMMV. It’s very early to make any concrete conclusions. The answer is time will tell.







300x240.png)