- Joined
- Jan 4, 2010
- Messages
- 3,138
I just read that Gene Hackman as well as his wife and their dog were found dead in their home today, and that foul play is not suspected.
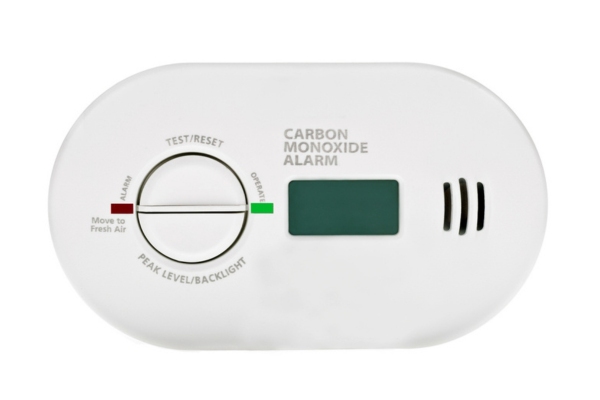
While no cause of death has been reported yet, an obvious possible cause is carbon monoxide poisoning. CO is odorless. It competes with oxygen to bind with the hemoglobin in your red blood cells. People basically die from lack of oxygen.
Whether that was the cause or not, this is a good time to remind folks that CO detectors can be life saving, and everyone should have at least one.
If you have one and have not changed the batteries this past year, consider doing it now.
While no cause of death has been reported yet, an obvious possible cause is carbon monoxide poisoning. CO is odorless. It competes with oxygen to bind with the hemoglobin in your red blood cells. People basically die from lack of oxygen.
Whether that was the cause or not, this is a good time to remind folks that CO detectors can be life saving, and everyone should have at least one.
If you have one and have not changed the batteries this past year, consider doing it now.








300x240.png)