- Joined
- Jun 8, 2008
- Messages
- 56,762
"
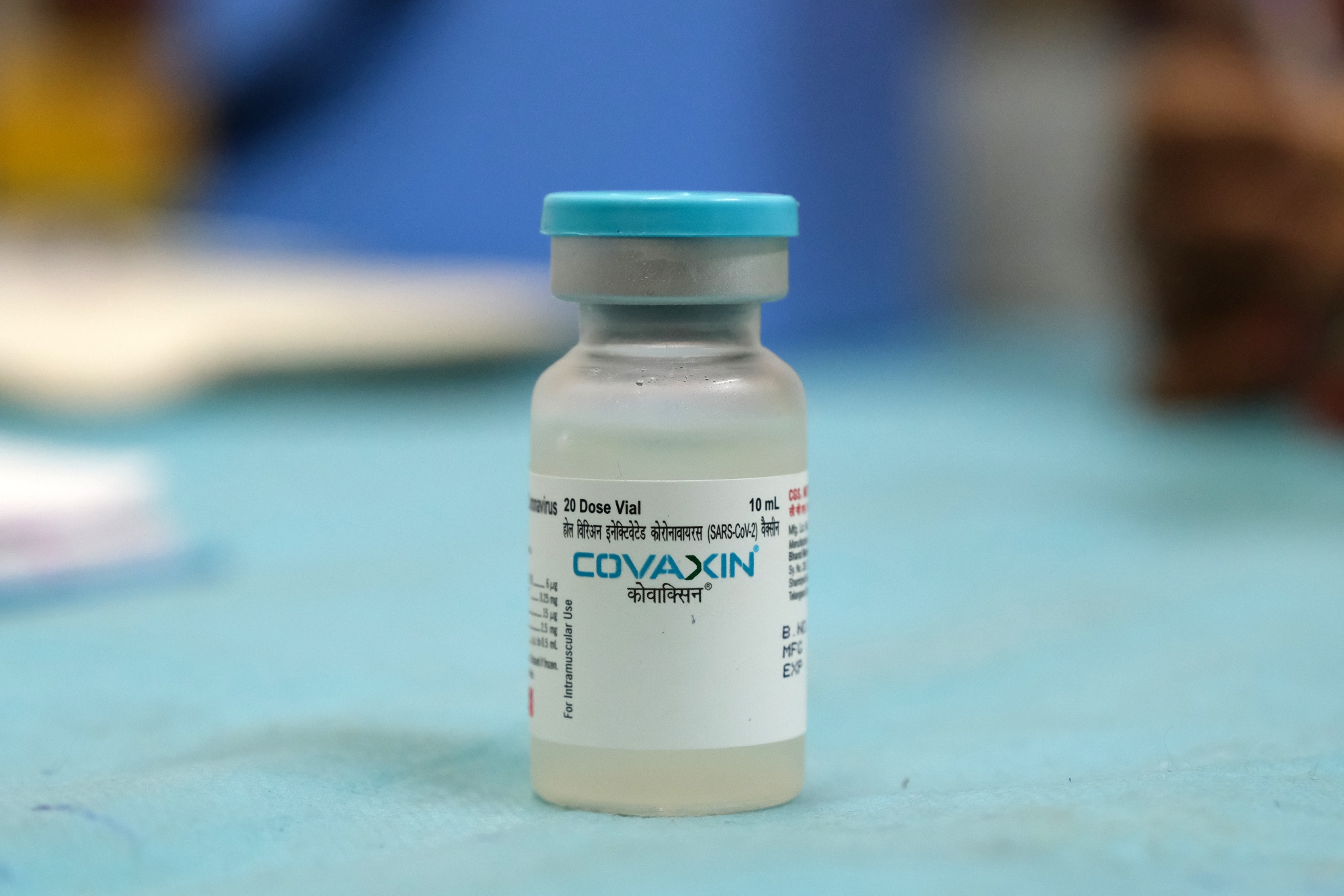
The U.S. is bracing for more staff shortages in the nation’s health care system after the Supreme Court made a critical decision on vaccine mandates. |
The ruling, which upholds the Biden administration’s requirement for millions of health care workers to be vaccinated against Covid, could wedge workers between opposing state and federal policies as hospitals wrestle with resistance among some staff. Many hospitals are already under strain from the biggest surge of Covid-19 patients since spring 2020. In New York City, there are simply not enough nurses to care for them all. |
While health care providers now have a clear mandate, U.S. businesses are largely on their own. The court’s decision to block the vaccine mandate for big companies means it’s now up to chief executives to decide when and how to pursue a “new normal.” |
In other developments: |
|
| : |












300x240.png)