- Joined
- Jun 8, 2008
- Messages
- 54,181
Can Paxlovid Improve Long COVID Symptoms?
— Harlan Krumholz, MD, discusses his ongoing study and novel approaches to clinical trials
by Jeremy Faust, MD, MS, MA, Editor-in-Chief, MedPage Today ; Emily Hutto, Associate Video Producer-
![author['full_name'] author['full_name']](https://clf1.medpagetoday.com/media/images/author/Faust_330px.png)
Jeremy Faust is editor-in-chief of , an emergency medicine physician at Brigham and Women's Hospital in Boston, and a public health researcher. He is author of the Substack column Inside Medicine. Follow -
![author['full_name'] author['full_name']](https://clf1.medpagetoday.com/media/images/author/EmilyHutto_188.jpg)
Emily Hutto is an Associate Video Producer & Editor for MedPage Today. She is based in Manhattan.
The following is a transcript of their remarks:
Faust: Hi, this is Jeremy Faust, editor-in-chief of MedPage Today.
We're going to talk about long COVID and Paxlovid. Does Paxlovid actually help people with diagnosed long COVID get better? This is a study that is being conducted -- there are several studies -- and one of the investigators on one of those studies is cardiologist and Yale School of Medicine outcomes researcher, Dr. Harlan Krumholz.
Harlan, great to see you.
Krumholz: It's great to see you, Jeremy.
Faust: Alright, so long COVID. You have been studying this and you're currently engaged in a randomized clinical trial. Can you tell us what you guys are looking at?
Krumholz: Sure. And when you say "you guys," let me just say I have the great privilege of working with Akiko Iwasakiopens in a new tab or window. Honestly for me, the ability to work with a renowned scientist like that in the lab who can bring insights to aniline biology is essential to this kind of research. I mean, I'm a clinical investigator, I'm an outcomes researcher. I really care whether or not we can produce knowledge that can tangibly improve people's lives, help them feel better, actually relieve the suffering.
But I recognize in a condition like this, unlike where I'm usually studying, like heart disease is fairly well-characterized, it's pretty mature. We still have a lot to learn, but I've never been in a situation where we've got a disease that is puzzling to most people. They don't understand the underlying mechanisms, it's not clear what the taxonomy is or what we're actually dealing with, and what an honor for me to be able to work with someone who can actually help provide insight into the underlying immunologic dimensions of this condition.
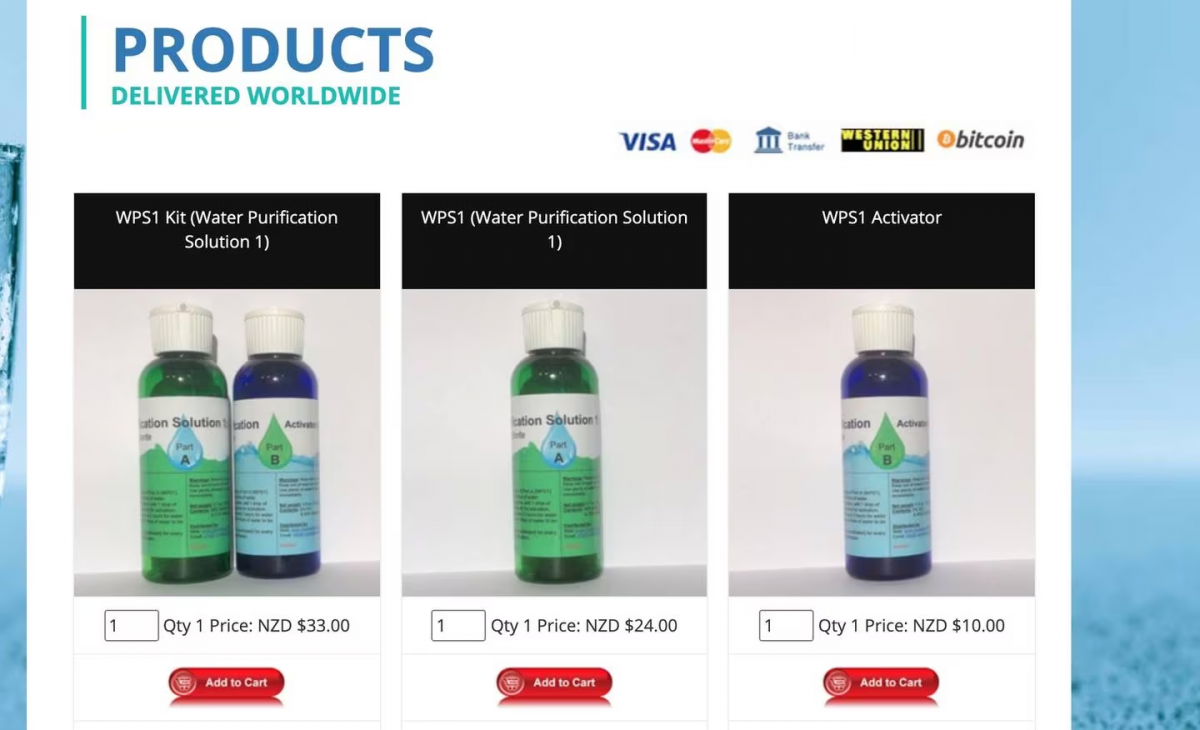
That plus we got a whole team of people, really talented individuals, and we came together and said, there are various different underlying causes potentially of long COVID. One of them is this idea of viral persistence, that people just never get rid of the virus and it continues to cause mischief in a wide variety of ways.
Let's try an antiviral, and there may be many choices in that. In part, it was because as we were in conversation with various groups. Pfizer was interested in seeing Paxlovid applied in this way and was willing to provide funding for us to do it and willing to provide the drug.
So for us it was an idea that, let's get started. Let's try to create a platform where we can do remarkable research in highly efficient ways, utilizing digital data, and really see if we can do a decentralized study -- one where people don't have to go to sites, build up that platform, and if we can start with Paxlovid, let's start.
That's what we did. We got out of the gates with a trial that would focus on using Paxlovid for 15 days in people highly symptomatic with long COVID and see whether or not we could learn anything.
Faust: Right. And that's the distinction that I just always have to myself be reminded of, which is this is not a study of people who have COVID right now in the first few days of illness, they're getting Paxlovid for a certain amount of time and then we look down 3, 6, 9, 12 months later to see if they got long COVID.
That is not what this is. This is for people who actually already have the diagnosis of long COVID, right?
Krumholz: That's right. That's exactly right.
Those studies are meritorious too, but they're prevention studies. Can we make an intervention early that lowers the risk of people ever developing something like long COVID? I'm interested in those. I think we all should be.
But there are lots of people out there who are suffering from the ravages of COVID throughout the course of the pandemic who 3 months or longer later are still having debilitating symptoms. For many of them, their lives have been unraveled.
The question is: what can we do to help them? What is going on with them to cause the kind of symptoms that they've got?
The "what" is, obviously, we're trying to see whether or not an antiviral Paxlovid can make a difference for people who are suffering from long COVID. But we thought, can we innovate the way that we do trials? The idea was, could we create a digital, decentralized, and democratized approach to doing a clinical trial in which we didn't need any sites. We're actually going direct to consumer, we're going straight to the people, one IRB [institutional review board], no site contracts. And what we're doing is enlisting people to fill out a questionnaire. If they qualify, we get them to integrate their medical records; we can review the records at a distance. If they qualify, we call them up, make sure what's in the record really reflects their reality, what they understand as their conditions and comorbidities, and do they qualify for this study.
If they qualify, we're off to the races -- we can randomize them, we ship [the] drug, we send people to their homes to get biospecimens that go to Akiko's lab; they do daily diaries on their device. We're in constant communication with them, a lot digital, some by phone. They're filling out surveys, the patient-reported outcome measures, and we're getting the feeds from their medical records to look at their healthcare utilization. And all the time, everything's being done from the convenience, largely, of their home; they don't have to leave. Many of these people are quite debilitated, tired, fatigued, and really don't have the financial resources. For those who are working hourly, it would be a big deal to have to take off half a day to go to a site, even to drive and use gas.
There are no clinical trial deserts in this study, because no matter where you live, you can be part of it. And we enrolled rapidly. The study, once we sort of worked out the kinks and the processes, is going extraordinarily well. I think it can be a means by which we can do highly efficient trials going forward that are really consumer-centric, participant-centric.
The other thing is, we don't call these people "subjects." They're our partners in the project. We're going to return results to them, we're going to give them access to investigators through town halls when we're finished, and we work hard to treat them with respect. We want them to give us like a net promoter score of five. Like, "Hey, I would brag to my friends that they should be in trials like this because they treat me well and I'm part of the team and we're on a mission together."
So yeah, we're really excited about how we did this and think that this can be a standard going forward.
Faust: I'm really interested in the idea of not knowing. One of the real successes of our COVID experience was the ACTIVopens in a new tab or window trial and the RECOVERYopens in a new tab or window trial in the U.K. where just a lot of things were tried and we said, "We're not smart enough to know which of these things is going to work. We just know that maybe among this group of 10, one thing will play out."
Do you feel like you have so many people who are interested here that you could throw in at some point a metformin arm or some other arm of the study, because Paxlovid is one thing, but there are other candidates?
Krumholz: Yeah, I think that's a really great question and a very important point.
We would be best off to do these kinds of platform trials where in the course of it we're testing 20 things. If it's an early study, then it's signal-finding. If you were really actually trying to test the hypothesis formally, it has to be powered appropriately. But there are enough people out there who are suffering who could be parts of these.
We really are moving too slowly. If we just do things one at a time, we're not going to learn fast enough to really solve this problem in the near future.
So I like what you're saying and I totally agree with it, and that in part was the idea behind how we built this platform. We wanted to be able to build this so that now if you've got five or six more things, if we can get the funding for it, why wouldn't you just build it in? We're all sitting ready to go.
Faust: Here we are coming into December of 2023 already and people are eager for results. When do you think we're going to get a readout from your study?
Krumholz: I think we'll finish up soon after the first of the year. I would say by June, I hope we'll be able to have a report out.
Our primary endpoint is 28 days with the PROMIS [Patient-Reported Measurement Information System]-29opens in a new tab or window physical function scale. It's sort of a net overall of how your physical health is; it's the change from baseline. But we're collecting a lot of other information on mental health and a whole range of other things that we'll learn from.
Again, like I said, it should be signal-finding. Who were responders, if there were any, and then we'll be able to not only characterize them from who they were clinically, demographically, and so forth, but because of the work that Akiko will do in the lab, we'll also say were there any baseline biomarkers that were indicative of people who were likely to respond to the treatment, and that could advance our understanding of the underlying mechanism, but also maybe be able to help us figure out who should be treated and who's likely to benefit.
Faust: Harlan Krumholz, thanks so much for joining us.
Krumholz: Thanks, Jeremy. It's great to talk to you.




300x240.png)