- Joined
- Jun 8, 2008
- Messages
- 54,265
"

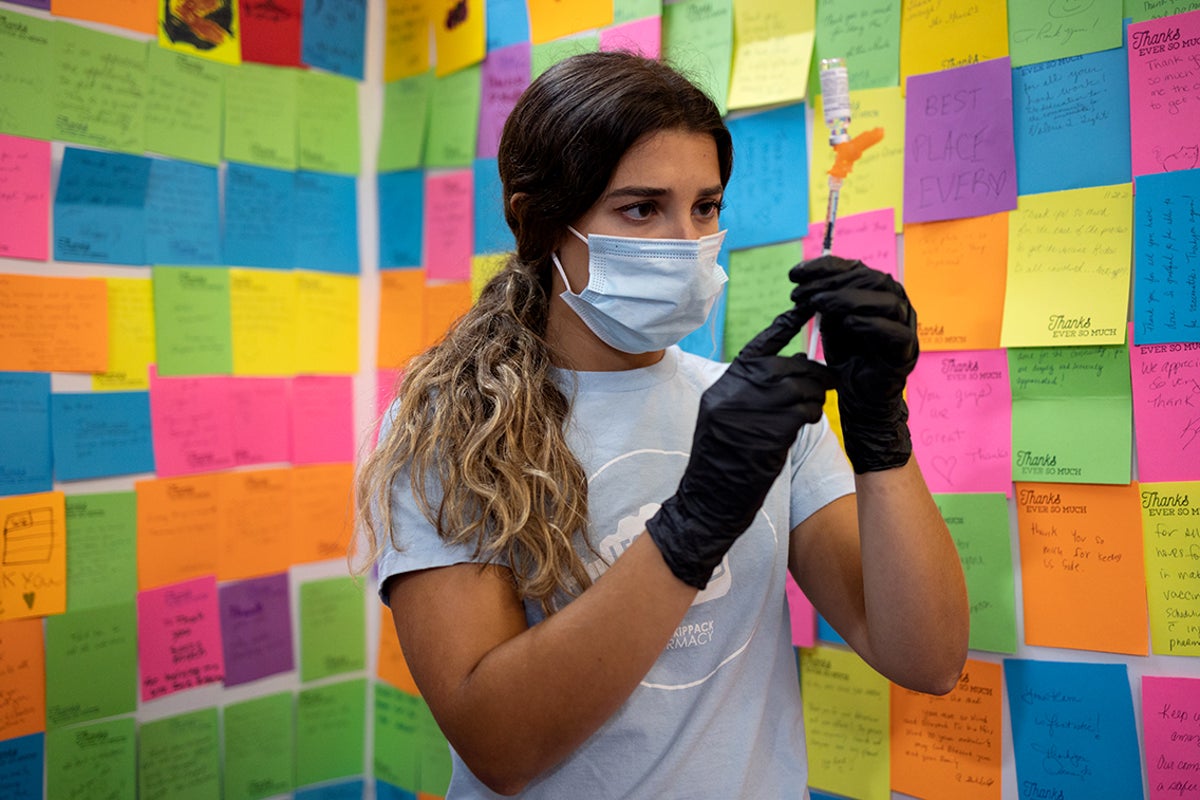
Maternal COVID vaccination in pregnancy protected young infants against Omicron-associated hospitalization, but few women actually receive the vaccine during pregnancy, according to new data from the CDC.
At least one maternal vaccine dose had an effectiveness of 54% (95% CI 32-6 against COVID-related hospitalization among infants younger than 3 months of age, and an effectiveness of 35% (95% CI 15-51) for infants younger than 6 months, reported researchers led by Regina Simeone, PhD, of CDC's National Center for Immunization and Respiratory Diseases in Atlanta, in the Morbidity and Mortality Weekly Reportopens in a new tab or window (MMWR).
against COVID-related hospitalization among infants younger than 3 months of age, and an effectiveness of 35% (95% CI 15-51) for infants younger than 6 months, reported researchers led by Regina Simeone, PhD, of CDC's National Center for Immunization and Respiratory Diseases in Atlanta, in the Morbidity and Mortality Weekly Reportopens in a new tab or window (MMWR).
Newborns are ineligible for COVID vaccination until 6 months of age, but are at high risk for severe outcomes from the virus. In fact, infants younger than 6 months have the highest COVID-associated hospitalization rates outside of seniors.
The case-control study from Simeone and colleagues spanned March 2022 to May 2023 and included 716 hospitalized infants under 6 months of age at 26 hospitals across 20 states in the Overcoming COVID-19 Network. In total, 78% of the 377 infants hospitalized and confirmed to have COVID-19 were babies whose mothers were unvaccinated. Most of the infants hospitalized for COVID-19 were previously healthy (77%), and critical illness occurred in 13%.
"Maternal vaccination, including receipt of a third dose during pregnancy, has been associated with reduced risk for infant hospitalization. Further, maternal vaccination during pregnancy has not been associated with increased risk for adverse pregnancy and infant outcomes," noted Simeone and co-authors.
Their findings were released alongside two other MMWRs showing lower rates of COVID vaccine uptakeopens in a new tab or window during pregnancy compared with other vaccinations recommended by the Advisory Committee on Immunization Practices (ACIP), and provider differencesopens in a new tab or window when it came to recommending the vaccines for this patient population.
Vaccine Uptake in Pregnancy, Hesitancy
A survey study led by Hilda Razzaghi, PhD, of CDC's National Center for Immunization and Respiratory Diseases, found that pregnant women were less likely to get the COVID vaccine during the 2022-2023 flu season compared with other vaccines recommended by ACIP during pregnancy to reduce the risk of pertussisopens in a new tab or window and influenza among women and their infants.
In an online survey conducted this year from March 28 to April 16 among more than 1,800 pregnant women, 27.3% said they received the bivalent COVID booster, as compared with 47.2% for the annual flu shot and 55.4% for the tetanus toxoid, diphtheria toxoid, and acellular pertussis (Tdap) vaccine.
Looking at the COVID shot specifically, women were nine times more likely to receive a bivalent booster if a provider recommended it (63.2% vs 6.8% when a provider did not).
Razzaghi's team also found an increase in flu vaccine hesitancy during pregnancy for the 2022-2023 season (24.7% very hesitant) versus prior seasons (17.2% in 2021-2022 and 17.5% in 2019-2020) and for Tdap vaccination as well (19.8% vs 14.7% and 15.1%, respectively).
In the study, hesitancy for these recommended vaccines was higher in Black versus white women, according to the researchers, who added that prioropens in a new tab or window studiesopens in a new tab or window have shown that pregnant Black women are less likely to receive vaccine recommendations from their provider.
"Maternal vaccination coverage remains suboptimal," Razzaghi and co-authors wrote. "Culturally relevant vaccination recommendations from health care providers are critical to improving vaccination coverage, decreasing persistent disparities in vaccination coverage, combatting increases in vaccine hesitancy observed since the start of the COVID-19 pandemic, and reducing adverse maternal and infant illness and associated complications including death from these three vaccine-preventable diseases."
Provider Influence
Survey data from healthcare providers found that ob/gyns were the most likely to recommend COVID-19 vaccination to their pregnant patients, Mehreen Meghani, MPH, also of the National Center for Immunization and Respiratory Diseases, and colleagues detailed.
Of the 1,538 providers surveyed who cared for pregnant patients, ob/gyns were most likely to recommend the COVID vaccine (94.2%), followed by pediatricians (90.4%) and family practitioners or internists (82.1%), with nurse practitioners (NPs)/physician assistants (PAs) being least likely to recommend it (76.0%).
When asked how important it was for women of reproductive age to stay up to date with COVID vaccination, 80.8% of the ob/gyns said it was very important, as compared with 78.8% of pediatricians, 69.1% of family practitioners or internists, and 55.6% of the NPs/PAs.
"One in five providers felt that it was only somewhat important that women of reproductive age stay up to date with COVID-19 vaccination, despite evidence that these women delay vaccination or remain unvaccinated," the study authors pointed out.
Providers who already offered Tdap and flu-shot vaccinations were more likely to offer or administer COVID shots as well.
These findings came from the Fall 2022 DocStyles survey. Most of the 1,752 responders were family practitioners or internists (57.2%), while pediatricians, ob/gyns, or NPs/PAs each made up 14.3% of the study sample. A majority of the providers were male (55.8%), and more than 60% had practiced for more than 10 years and worked in an outpatient setting.
Most of the providers in the study offered or administered the COVID-19 vaccine (53.5%), the flu shot (80.7%), and Tdap vaccination (71.9%) at their practice, though only 39.7% of ob/gyns offered the COVID vaccine.
"
COVID Vax in Pregnancy Protects Young Infants Against Omicron
— But only about one-fourth of pregnant women reported getting the vaccine
by Ian Ingram, Managing Editor, MedPage Today October 2, 2023
Maternal COVID vaccination in pregnancy protected young infants against Omicron-associated hospitalization, but few women actually receive the vaccine during pregnancy, according to new data from the CDC.
At least one maternal vaccine dose had an effectiveness of 54% (95% CI 32-6
Newborns are ineligible for COVID vaccination until 6 months of age, but are at high risk for severe outcomes from the virus. In fact, infants younger than 6 months have the highest COVID-associated hospitalization rates outside of seniors.
The case-control study from Simeone and colleagues spanned March 2022 to May 2023 and included 716 hospitalized infants under 6 months of age at 26 hospitals across 20 states in the Overcoming COVID-19 Network. In total, 78% of the 377 infants hospitalized and confirmed to have COVID-19 were babies whose mothers were unvaccinated. Most of the infants hospitalized for COVID-19 were previously healthy (77%), and critical illness occurred in 13%.
"Maternal vaccination, including receipt of a third dose during pregnancy, has been associated with reduced risk for infant hospitalization. Further, maternal vaccination during pregnancy has not been associated with increased risk for adverse pregnancy and infant outcomes," noted Simeone and co-authors.
Their findings were released alongside two other MMWRs showing lower rates of COVID vaccine uptakeopens in a new tab or window during pregnancy compared with other vaccinations recommended by the Advisory Committee on Immunization Practices (ACIP), and provider differencesopens in a new tab or window when it came to recommending the vaccines for this patient population.
Vaccine Uptake in Pregnancy, Hesitancy
A survey study led by Hilda Razzaghi, PhD, of CDC's National Center for Immunization and Respiratory Diseases, found that pregnant women were less likely to get the COVID vaccine during the 2022-2023 flu season compared with other vaccines recommended by ACIP during pregnancy to reduce the risk of pertussisopens in a new tab or window and influenza among women and their infants.
In an online survey conducted this year from March 28 to April 16 among more than 1,800 pregnant women, 27.3% said they received the bivalent COVID booster, as compared with 47.2% for the annual flu shot and 55.4% for the tetanus toxoid, diphtheria toxoid, and acellular pertussis (Tdap) vaccine.
Looking at the COVID shot specifically, women were nine times more likely to receive a bivalent booster if a provider recommended it (63.2% vs 6.8% when a provider did not).
Razzaghi's team also found an increase in flu vaccine hesitancy during pregnancy for the 2022-2023 season (24.7% very hesitant) versus prior seasons (17.2% in 2021-2022 and 17.5% in 2019-2020) and for Tdap vaccination as well (19.8% vs 14.7% and 15.1%, respectively).
In the study, hesitancy for these recommended vaccines was higher in Black versus white women, according to the researchers, who added that prioropens in a new tab or window studiesopens in a new tab or window have shown that pregnant Black women are less likely to receive vaccine recommendations from their provider.
"Maternal vaccination coverage remains suboptimal," Razzaghi and co-authors wrote. "Culturally relevant vaccination recommendations from health care providers are critical to improving vaccination coverage, decreasing persistent disparities in vaccination coverage, combatting increases in vaccine hesitancy observed since the start of the COVID-19 pandemic, and reducing adverse maternal and infant illness and associated complications including death from these three vaccine-preventable diseases."
Provider Influence
Survey data from healthcare providers found that ob/gyns were the most likely to recommend COVID-19 vaccination to their pregnant patients, Mehreen Meghani, MPH, also of the National Center for Immunization and Respiratory Diseases, and colleagues detailed.
Of the 1,538 providers surveyed who cared for pregnant patients, ob/gyns were most likely to recommend the COVID vaccine (94.2%), followed by pediatricians (90.4%) and family practitioners or internists (82.1%), with nurse practitioners (NPs)/physician assistants (PAs) being least likely to recommend it (76.0%).
When asked how important it was for women of reproductive age to stay up to date with COVID vaccination, 80.8% of the ob/gyns said it was very important, as compared with 78.8% of pediatricians, 69.1% of family practitioners or internists, and 55.6% of the NPs/PAs.
"One in five providers felt that it was only somewhat important that women of reproductive age stay up to date with COVID-19 vaccination, despite evidence that these women delay vaccination or remain unvaccinated," the study authors pointed out.
Providers who already offered Tdap and flu-shot vaccinations were more likely to offer or administer COVID shots as well.
These findings came from the Fall 2022 DocStyles survey. Most of the 1,752 responders were family practitioners or internists (57.2%), while pediatricians, ob/gyns, or NPs/PAs each made up 14.3% of the study sample. A majority of the providers were male (55.8%), and more than 60% had practiced for more than 10 years and worked in an outpatient setting.
Most of the providers in the study offered or administered the COVID-19 vaccine (53.5%), the flu shot (80.7%), and Tdap vaccination (71.9%) at their practice, though only 39.7% of ob/gyns offered the COVID vaccine.
"











![author['full_name'] author['full_name']](https://clf1.medpagetoday.com/media/images/author/EShort_188.jpg)










![author['full_name'] author['full_name']](https://clf1.medpagetoday.com/media/images/author/ESusman_188.jpg)






300x240.png)